The Menstrual Cycle Explained: Key Phases and Fertility Signals

Understanding the menstrual cycle is essential for anyone seeking to optimize fertility and reproductive health. The cycle is a complex monthly process, signaling when the body is most fertile and helping to identify potential issues that may affect conception. Key Phases of the Menstrual Cycle The menstrual cycle typically consists of three main phases, each playing a vital role in reproductive health: Fertility Signals Throughout the Cycle Recognizing bodily signals during each phase helps identify fertility windows: Support from Fertility Specialists Whether planning for pregnancy or seeking to understand reproduction, consulting fertility specialists like those at Ziva Fertility can provide expert guidance. Clinics offer cycle tracking, diagnostic services, and personalized fertility solutions. For professional support, contact Ziva Fertility at 91 00 00 2737, or visit their clinics at Manikonda and Sanathnagar. More details are available at zivafertility.com
The Fertility Journey: What to Expect When You Start Trying

Embarking on the journey to parenthood is an exciting and emotional experience. Many couples are unsure about what to expect when they start trying to conceive. Understanding the key stages and processes involved can help reduce anxiety and empower you to make informed choices. What to Expect on Your Fertility Journey The fertility journey often starts with hopeful anticipation, but it can come with questions and concerns. It’s important to recognize that everyone’s experience is unique, and the path to pregnancy may include both natural conception and possible assisted reproductive technologies. In Vitro Fertilization (IVF) Process The image summarises a common assisted reproductive process—IVF. Here’s a step-by-step overview: Support and Resources Fertility clinics like Ziva Fertility provide end-to-end support, offering diagnostics, counseling, and advanced treatments tailored to your needs. Whether you’re just starting or exploring options like IVF, their compassionate team can guide you every step of the way. For personalized support, contact Ziva Fertility at 91 00 00 2737 or visit their clinics at Manikonda and Sanathnagar. Learn more at zivafertility.com
Understanding Your Fertility Window: How to Track Ovulation
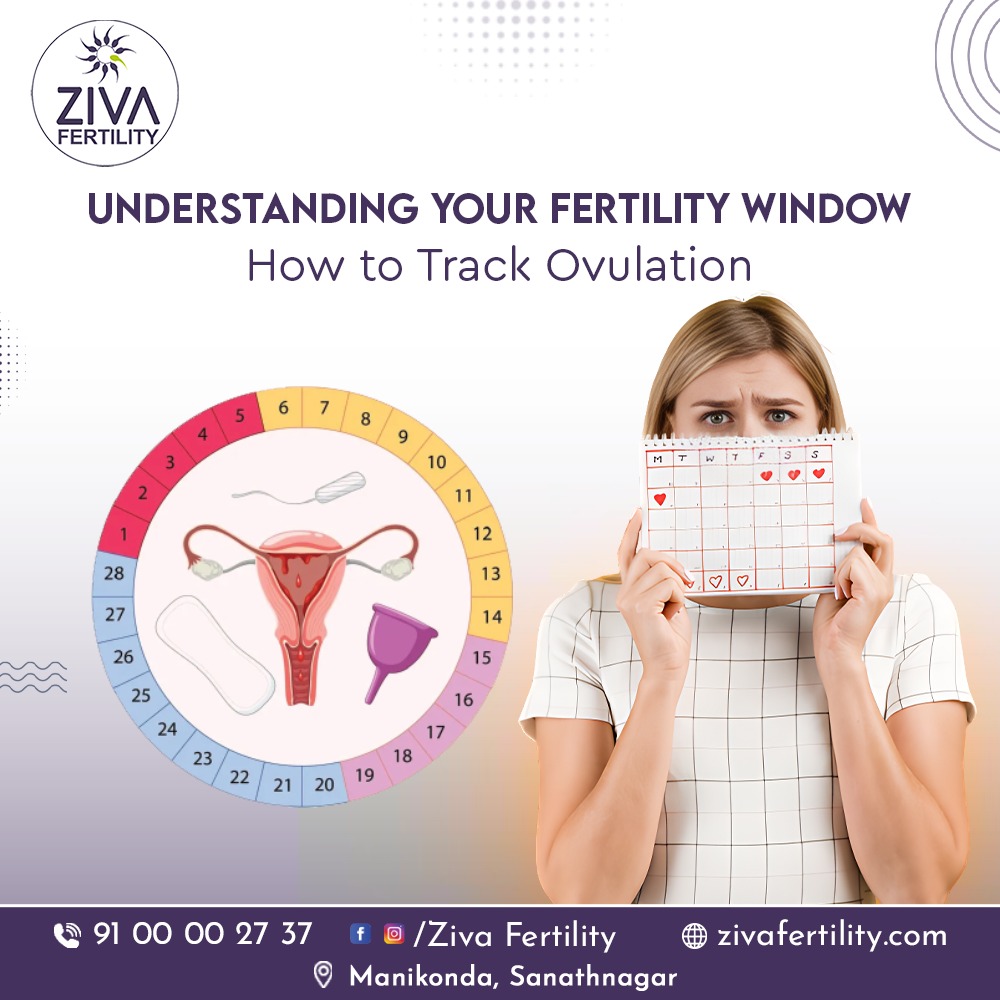
For couples trying to conceive, understanding the fertility window can make a significant difference. Your fertility window refers to the few days in your menstrual cycle when conception is most likely to occur. Knowing how to identify and track ovulation helps you plan for pregnancy more effectively. What Is Ovulation? Ovulation is the process when a mature egg is released from the ovary and travels down the fallopian tube, ready for fertilization. This usually happens about 14 days before your next period begins, but the timing can vary for each woman. Why Tracking Ovulation Matters Understanding when you ovulate helps you identify your most fertile days. Intercourse during this period increases your chances of conception. Tracking ovulation is especially helpful for couples who have been trying for a while or those with irregular cycles. How to Track Ovulation There are several methods to help you find your fertility window: Understanding the Fertility Window The fertile window typically includes the five days before ovulation and the day of ovulation itself. Sperm can live up to 5 days in the female reproductive system, so planning intercourse during these days increases conception chances. When to Seek Medical Advice If you’ve been tracking ovulation and trying to conceive for over a year (or 6 months if you’re over 35) without success, it’s best to consult a fertility specialist. Conditions like PCOS, thyroid imbalances, or hormonal irregularities can affect ovulation. At ZIVA Fertility At ZIVA Fertility, we help you understand your body better and guide you with personalized fertility assessments. Our specialists provide advanced ovulation tracking, fertility tests, and treatment options to support your journey toward parenthood.
How Age Affects Fertility: What You Should Know in Your 20s, 30s, and 40s

Fertility is influenced by many factors, but age is one of the most significant. As people progress through their 20s, 30s, and 40s, fertility naturally changes, affecting the chances of conceiving and leading to a healthy pregnancy. Understanding this relationship can help individuals and couples make informed decisions about family planning and reproductive health. Fertility in Your 20s During the 20s, fertility is generally at its peak. Women have the highest quantity and quality of eggs, and men typically have optimal sperm health. Most couples in this age group conceive within a year of trying, but it’s still important to prioritize overall reproductive health by maintaining a balanced lifestyle. Fertility in Your 30s By the early 30s, fertility begins to gradually decline. The number and quality of eggs start to decrease, especially after age 35. Many couples conceive without intervention, but the likelihood of fertility issues becomes more noticeable. Regular check-ups and fertility assessments are recommended if conception does not occur after six months to a year of trying. Fertility in Your 40s Fertility declines more rapidly in the 40s. The chances of natural conception are lower, and the risk of pregnancy complications increases. However, with advances in fertility treatments and medical support, many individuals and couples successfully have children in their 40s. Consulting a fertility specialist becomes increasingly important at this stage. What You Should Know For more information and personalized fertility support, you can contact Ziva Fertility at 91 00 00 27 37 or visit their clinics at Manikonda and Sanathnagar. Further details are available on their website: zivafertility.com
Pregnant? Have Your COVID-19 Vaccines!
Pregnancy is a beautiful and special time, but it also requires extra care to protect both mother and baby. Receiving your COVID-19 vaccines during pregnancy is crucial for your health and your unborn child’s well-being. Why COVID-19 Vaccination is Important in Pregnancy What to Expect from the Vaccine Stay Protected, Stay Healthy COVID-19 infection can pose serious risks during pregnancy, so getting vaccinated is a vital step to safeguard your health and the health of your baby. Talk to your healthcare provider about receiving the vaccine if you are pregnant or planning to become pregnant. Conclusion Taking your COVID-19 vaccines during pregnancy is one of the best decisions you can make to protect yourself and your unborn child from severe illness. Vaccination offers peace of mind and helps ensure a healthier pregnancy journey.
Blocked Fallopian Tubes? IVF Can Be an Effective Option to Conceive

Blocked fallopian tubes are a common cause of female infertility that can prevent the egg and sperm from meeting, making natural conception difficult or impossible. The fallopian tubes play a critical role in fertilization and the transport of the fertilized egg to the uterus. What Causes Fallopian Tube Blockages? Symptoms of Blocked Fallopian Tubes Many women do not experience symptoms until they encounter infertility. Some may have: Diagnosis of Blocked Tubes Treatment Options Why Choose IVF with ZIVA Fertility? At ZIVA Fertility, we specialize in advanced treatments like IVF that help couples overcome fallopian tube blockages and achieve pregnancy. Our expert team offers compassionate care, proven success rates, and personalized treatment plans designed to meet your unique fertility needs. Take the Next Step If you suspect or know you have blocked fallopian tubes, consult with ZIVA Fertility for a comprehensive evaluation and guided treatment options. IVF could be the path to your parenthood dreams.
Suffering with Ovulation Problems? Start Your Parenthood Journey at ZIVA Fertility

Ovulation problems are among the most common causes of infertility in women. When ovulation is irregular or absent, it prevents the release of eggs necessary for conception. If you’re struggling with ovulation issues, it’s important to seek expert care to improve your chances of pregnancy. Common Causes of Ovulation Problems Symptoms of Ovulation Problems Treatment Options Why Choose ZIVA Fertility? At ZIVA Fertility, we provide personalized fertility assessments and treatments tailored to address ovulation problems effectively. Our experienced specialists combine advanced technology with compassionate care to help you achieve your dream of parenthood. Take the First Step Today Don’t let ovulation issues keep you from starting or growing your family. Book your consultation at ZIVA Fertility and begin your journey to parenthood with confidence.
Low Sperm Count: A Common Cause of Infertility in Men and the Role of ICSI Treatment

Low sperm count, medically known as oligospermia, is one of the leading causes of male infertility. It occurs when the number of sperm in the semen is below the threshold needed for natural conception, usually fewer than 15 million sperm per milliliter of semen. Understanding Low Sperm Count What Is ICSI and How Does It Help? Intracytoplasmic Sperm Injection (ICSI) is an advanced assisted reproductive technology specifically designed to overcome male infertility due to low sperm count or poor sperm quality. During ICSI: Effectiveness of ICSI for Low Sperm Count Conclusion Low sperm count is a common infertility factor that can be addressed with modern reproductive technologies. ICSI offers an effective solution by directly assisting fertilization, significantly improving pregnancy chances for affected couples.
Early Signs and Symptoms of Pregnancy: What to Watch For

Pregnancy brings many exciting changes, some of which can start even before you realize you’re expecting. Recognizing the early signs and symptoms can help you confirm pregnancy sooner and begin important prenatal care. Common First Signs of Pregnancy Other Possible Early Symptoms What to Do If You Suspect Pregnancy If you experience these symptoms and suspect you might be pregnant, taking a home pregnancy test and consulting your healthcare provider for confirmation and prenatal care is the next step. Conclusion While pregnancy symptoms can vary widely between women, being aware of these early signs can prepare you emotionally and physically for the incredible journey ahead.
9 Tips to Beat Low Sperm Count and Boost Fertility

Low sperm count, or oligospermia, can be a major hurdle for couples trying to conceive. Fortunately, there are many effective lifestyle changes and treatments that can help increase sperm count and improve overall fertility. Here are nine essential tips: 1. Don’t Smoke Smoking damages sperm DNA, reduces motility, and lowers sperm count. Quitting smoking can significantly improve sperm health. 2. Avoid Heat High temperatures can harm sperm production. Avoid hot tubs, saunas, tight underwear, and prolonged laptop use on your lap. 3. Steer Clear of Illicit Drugs Substances like anabolic steroids, cocaine, and marijuana negatively affect sperm quality and quantity. 4. Manage Stress Chronic stress increases cortisol, which can reduce testosterone and impair sperm production. Use relaxation techniques like meditation, exercise, or counseling. 5. Limit or Abstain from Alcohol Excessive alcohol intake lowers sperm count and motility. Reducing or eliminating alcohol can boost fertility. 6. Use Evergreen Formula for Men to Boost Sperm Certain supplements containing antioxidants, zinc, folic acid, and CoQ10 support sperm health. Consult your doctor before starting any supplements. 7. Avoid Exposure to Pesticides, Heavy Metals, and Toxins Environmental toxins harm sperm quality. Use protective gear if exposed to chemicals at work, and choose organic foods when possible. 8. Avoid Foods That Contribute to Low Sperm Count Minimize processed foods, trans fats, and excessive sugar intake, which can worsen sperm health. 9. Maintain a Healthy Weight Both overweight and underweight can affect hormone balance and sperm production. A balanced diet and regular exercise help maintain optimal weight. Understanding Low vs. Normal Sperm Count Conclusion Improving sperm count is often possible through lifestyle adjustments, medical treatments, and sometimes assisted reproductive techniques. Early evaluation and action can dramatically improve fertility outcomes.
