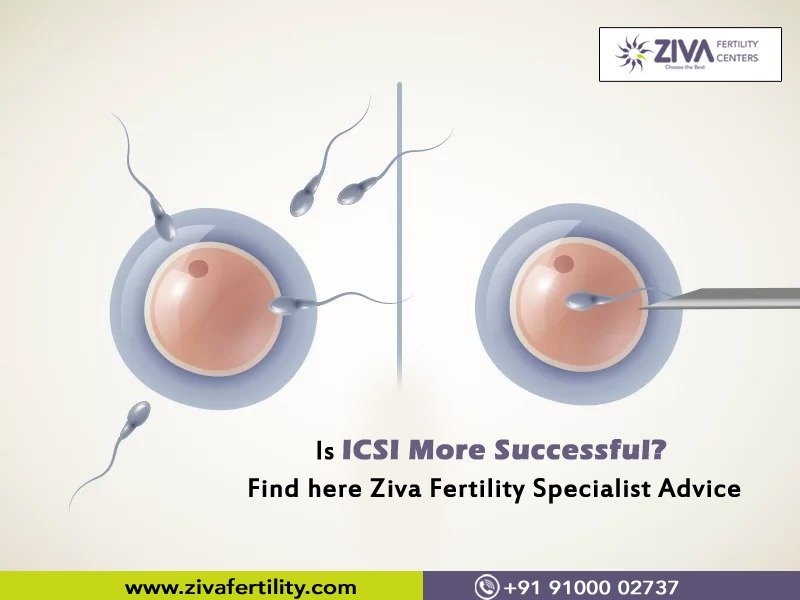
Many couples who cannot conceive children by natural means now have the boon of ARTs (Assisted Reproductive Techniques). Each ART technique is suitable for a particular cause of Infertility. Age, overall health, and cause of Infertility are determining factors in selecting a suitable ART. IVF, IUI, ICSI etc., have a success record. In this blog, we will understand the success of ICSI i.e. Intra-cytoplasmic Sperm Injection (ICSI). ICSI is a specific procedure used in In-Vitro Fertilization (IVF) cases. ICSI is recommended in male infertility cases like meager sperm count or abnormally poor sperm motility. A single sperm is injected into the egg to fertilize it. Since the sperm is directly injected into the egg, the chance of successful fertilization is significantly increased.
Why is ICSI more successful?
The combination of an IVF with ICSI has shown a much higher success rate than regular IVF. According to the American Society for Reproductive Medicine (ASRM), through the method of ICSI, around 50-80% of the eggs have been fertilized. In some cases, even when the sperm is directly injected into the egg, it may not fertilize it. After fertilization, a fetus is formed only when the egg attaches itself to the uterine lining.
When is ICSI most successful?
In a regular IVF, a large quantity of sperm is placed along with an egg. The hope is that one sperm will enter and fertilize the egg all by itself. In an ICSI-IVF procedure, there is sperm selection.
ICSI has the best success rate under the following scenarios:
- At least one unsuccessful IVF cycle. In an IVF, a good number of eggs may be retrieved, and sperm count also looks good, but fertilization does not happen. In these scenarios, the next IVF cycle is combined with an ICSI.
- When the male partner’s sperm count is as low as 1 or 2 mill/ ml, also known as Oligospermia
- Abnormally shaped sperm, also known as Teratozoospermia.
- The sperm in the semen has very poor motility, also known as Asthenozoospermia.
- If anti-sperm antibodies are present in the semen, which will damage the sperm and keep them from fertilizing the egg
- There is sperm production in the male partner, but this sperm is not present in the semen ejaculated. This happens due to a condition called vas deferens. In such cases, the sperm may be retrieved through testicular sperm extraction or TESE. The use of ICSI is necessary in the cases of TESE.
- In cases of using frozen sperm, if the thawed sperm don’t appear especially active, ICSI-IVF may be recommended.
- In cases of using frozen oocytes, eggshell hardening has been observed. The vitrification of eggs can sometimes cause the hardening of the eggshells. When the eggshell is hard, sperm may not naturally enter the egg, and in such cases, IVF with ICSI may help overcome this hurdle.
Reasons for ICSI’s success
- The main reason for the success of ICSI is that the sperm is injected directly into the egg. So this removes the uncertainty of whether the sperm has entered the egg.
- The embryologist has the chance to pick out the best sperm. A high-quality sperm is preselected and then inserted into the egg. This greatly enhances the chances of pregnancy.
If anyone suspects birth defects, please note that the chance of birth defects with IVF and ICSI are similar. However, the birth defects may not have anything to do with the procedure but are due to the couple’s infertility issues.
When is ICSI not recommended?
This is a matter of subjective discussion. However, below are a few of the cases where ICSI has not shown many results:-
Fewer eggs retrieved during IVF: In an IVF, after ovarian stimulation, eggs are retrieved. However, if there are less number of eggs, then why take the risk that they won’t get fertilized? In such cases, the research did not find that pregnancy or live birth rates improved with ICSI.
Unexplained Infertility: Doctors use ICSI to treat unexplained Infertility. Since we don’t know what is wrong, treating every possibility is a good action plan. But till now, research has not found that ICSI in the cases of unexplained infertility significantly improved live birth success rates.
Not every IVF needs an ICSI- Some reproductive endocrinologists practise an ICSI for every IVF. But for every 33 patients, only one has shown benefit from the routine use of IVF-ICSI.
ICSI Procedure in a nutshell
Just like IVF, ICSI is also done in a lab. So there is not much difference when compared to only IVF treatment. In an ICSI also, you’ll take ovarian stimulating drugs, and your doctor will monitor your progress with blood tests and ultrasounds. After growing good-sized follicles, you’ll have egg retrieval, where eggs are removed from your ovaries with a specialised, ultrasound-guided needle. On the same day, the male will provide a sperm sample. One can also use a sperm donor or previously frozen sperm at this stage.
After a good quality of eggs is retrieved, an embryologist will place the eggs in a unique culture. With the help of a microscope and a tiny needle, a single sperm will be injected into an egg. All the eggs retrieved will undergo the same insertion. After successful fertilization, if the embryos are healthy, an embryo or two will be transferred to your uterus via a catheter placed through the cervix two to five days after the retrieval.
We at ZIVA Fertility Clinics take informed decisions and always put the patient’s interests first. We will consider all aspects before recommending ICSI. Please visit our website https://zivafertility.com/ or reach us at +91-9100002737, +91-9392834024
Info@zivafertility.com